Janice
Much of Janice’s life has been dedicated to public service.
She left school to join an enrolled nursing programme and, after marrying and having three children, she went on to achieve a Bachelor of Nursing and ultimately a post graduate diploma in Health Science. Nursing, in some form or another, has been part of Janice’s life for the best part of 40 years.

Janice is a picture of good health but her charisma, warm smile and sparkling, bright eyes hide a horrible truth. The 61-year-old has lung cancer which has metastasised behind her right eye. She becomes emotional when she talks about her prognosis. It is grim. However, her tears are for her husband and her three children. It is her family she is most concerned about.
“You don’t want to be a burden to your kids, and suddenly that is the reality. It’s going to happen, and it’s every mother’s worst nightmare.”
Janice, a mother of three and a grandmother to two busy preschoolers, works for Corrections Waitaha at Rolleston Prison in Christchurch. She is focused primarily on trying to improve mental health among prisoners using talk-based therapy.
“My career developed to a point where I wanted to look at the body and mind together. You need to see the bigger picture and that can help you understand why someone is unwell.”

“I love it. It’s just me and the prisoner. I don’t ask what they’ve done or why they’re in there. I just deal with their reality.”
“We talk about their lives, how their household functioned, and what triggers their anxiety. These men have no control over their lives in prison, but it’s in their control to tell me their story. I think it’s sometimes easier talking to someone who isn’t judging them and not part of the system that confines them. I’m just there to listen and to help guide them.”
Janice has spent years working in our health system, nursing, and caring for others. It is a system, she says, that she has always believed in.

In 2021, Janice developed a niggly cough and sought help from her GP in the middle of the year. She was told it was reflux and was prescribed 20ml of an antacid. One month later, the dose was increased to 40ml but there was still no improvement. Janice kept pushing for a more thorough examination and was eventually granted a chest x-ray in September.
“The x-ray didn’t really pick up a lot. It looked like a small pocket of something, or perhaps an infection. They didn’t know what it was.”
The next step was a CT scan. Janice’s name went on the non-urgent list.
“It was stressful. I knew something wasn’t right, so every delay just added to the anxiety….”
Eventually, Janice had a CT scan on the 22nd of November. The next day, a GP phoned her.
“They wanted to see me in person but because of Covid, they couldn’t. So, they just told me over the phone. It must have been hard for them too. They said it looks like you have lung cancer, and I think I thanked them for telling me and then I hung up and called my husband.”
Once Paul was home, Janice says she phoned her children. Janice’s voice breaks again.
“It was hideous…. these days I try and keep as much of it from the kids as I can.”

One week later, an urgent bronchoscopy proved fruitless – it came back clear of cancer. Janice then went for a guided biopsy on the 23rd December which finally gave her a confirmed diagnosis. She had Stage 4 Non-Small Cell Lung Cancer (NSCLC). Janice knew it was moving quickly.
She was told her cancer was incurable, so she would be transferred from the Respiratory Team to the Oncology Team at Christchurch Public Hospital. They would test for a gene mutation and specialists would then determine the best line of treatment for Janice.
In some cases, modern, targeted immunotherapies can stunt tumour growth, and elongate a patient’s life. Janice was told she would be seen by Oncology within the next 10 days.
Tragically for Janice, the weeks and months that followed became a battle to survive.
“I felt like I was being left to die. Everything was a fight. Every appointment…. it’s hard to describe. It was just a battle to get help. Every step was a challenge.”

“They would test for one mutation, we would wait for the result and then they would call and say ‘you don’t have that mutation’ and so I’d have to wait until they tested for another mutation.”
More than four months had passed since Janice had presented to her GP, and she was still waiting for tests to determine her treatment plan. In the meantime, Janice’s health was declining. On New Year’s Eve, her sight began to go in her right eye. Unable to get an appointment, she went to the Emergency Department at Christchurch Hospital.
“…and they found a second mass behind my right eye.”
Janice says she feels sorry for the young specialist who had to break the news to her.
“He was upset too. He was a young man. It was just awful for everyone.”
Janice went home and over the coming days she developed a growing unease that no-one had been in contact with her, and she still didn’t have a treatment plan to arrest the cancer.
“And that’s when it began to get really soul-destroying in the hospital system.”

On the 12th of January, Janice was at Christchurch Public Hospital in the Ophthalmology department having a follow up examination on her eye. Paul, in the meantime, went to Oncology to find out why Janice still didn’t have an appointment. They gave him an honest answer.
“The Practice Manager told him they were so overwhelmed with work that it would be another five or six weeks before I could see an oncologist. She advised us to go private.”
“They also apologised for a letter that I would be sent from the DHB…..”
The Practice Manager explained the letter was a Ministry of Health requirement. It would state that Janice was on a waiting list for Oncology, and that she would receive an appointment by the 6th of April. That was still three months away.
“She said the letter upsets a lot of people….it was in the mailbox when we got home.”
Two days later, Janice had CT eye and body scans but “…Paul and I started saying ‘what’s next, what’s next, what’s next” ….and by this stage we were well into the New Year.”
The process dragged on for months and like so many vulnerable New Zealanders who have spoken to The Medicine Gap, Janice says she didn’t have the energy to fight the system.
“I couldn’t have fought them if I tried.”

In January, five months after her x-ray, Janice was told her cancer didn’t have a mutation. Her only option on the public health system was palliative chemotherapy, but there was no proactive plan or urgency applied to her treatment.
“I felt like everyone knew my cancer was more advanced, so it just didn’t matter anymore.”
Janice struggles to talk about the hospital system without becoming upset.
“I have worked in our health system for so long helping others and believing so strongly that it was a good system. I don’t want to believe that it doesn’t work because my entire career has been built on it. But when I needed the system, it didn’t work for me. It just didn’t.”
Janice says Paul got on the phone and “just kept calling”.
“It is pure survival, and I had to go against everything near and dear to me. It’s not the way I do business, and suddenly people were being asked to fit me in or find a way to treat me. I hated it. It is not me.”
Eventually, through friends and family, they found a specialist who made space for Janice and provided her with radiotherapy on her eye and chest “to slow things down”.
“He was a very nice man who did me a favour and offered me radiation.”

Given the delays in the public health system, Janice met with a private oncologist. It became clear that to extend her life, she would need to access the unfunded immunotherapy drug, Keytruda as part of a treatment plan that included chemotherapy. However, because Janice was being treated by a private clinic, she could no longer access chemotherapy through the DHB. She would have to pay for both. It would cost $110k for a year of private treatment.
“It’s a catch-22. You either face a long delay and get chemotherapy through the DHB, or you access it now and pay for the whole lot.”
On top of that, Janice would have to pay to have Keytruda administered through a private clinic. If the public health system doesn’t fund a modern treatment, they won’t support a patient to have it administered at a hospital.
Keytruda is available on a cost-sharing patient programme in New Zealand at a capped price of $60,000. But the Government applies GST to every medicine it doesn’t fund. In the case of Keytruda, it adds $9,000 to the bill.
It is a cruel irony that at a time when New Zealand is desperately short of nurses, Janice has to pay for the drugs to keep her alive and at work.

Every day, five New Zealanders die from lung cancer. It remains New Zealand’s biggest cancer killer, but we don’t fund the most effective drug to treat it.
Janice had no option but to cash in her life insurance policy to pay for Keytruda. She feels fortunate that she could find a way to pay for her treatment but says it will impact her family later in life. Keytruda doesn’t cure cancer, but it does elongate life.
Janice, tragically, feels a sense of guilt for using the money to help her live.
“I had always thought that money would be for my grandchildren. For their future. I was just so upset that I had to use it to try and stay alive.”
In the last month, Janice has ceased treatment and is focused on living well with the time she has left. Quality of life is important to her, and some cancer treatments can trigger challenging side-effects.
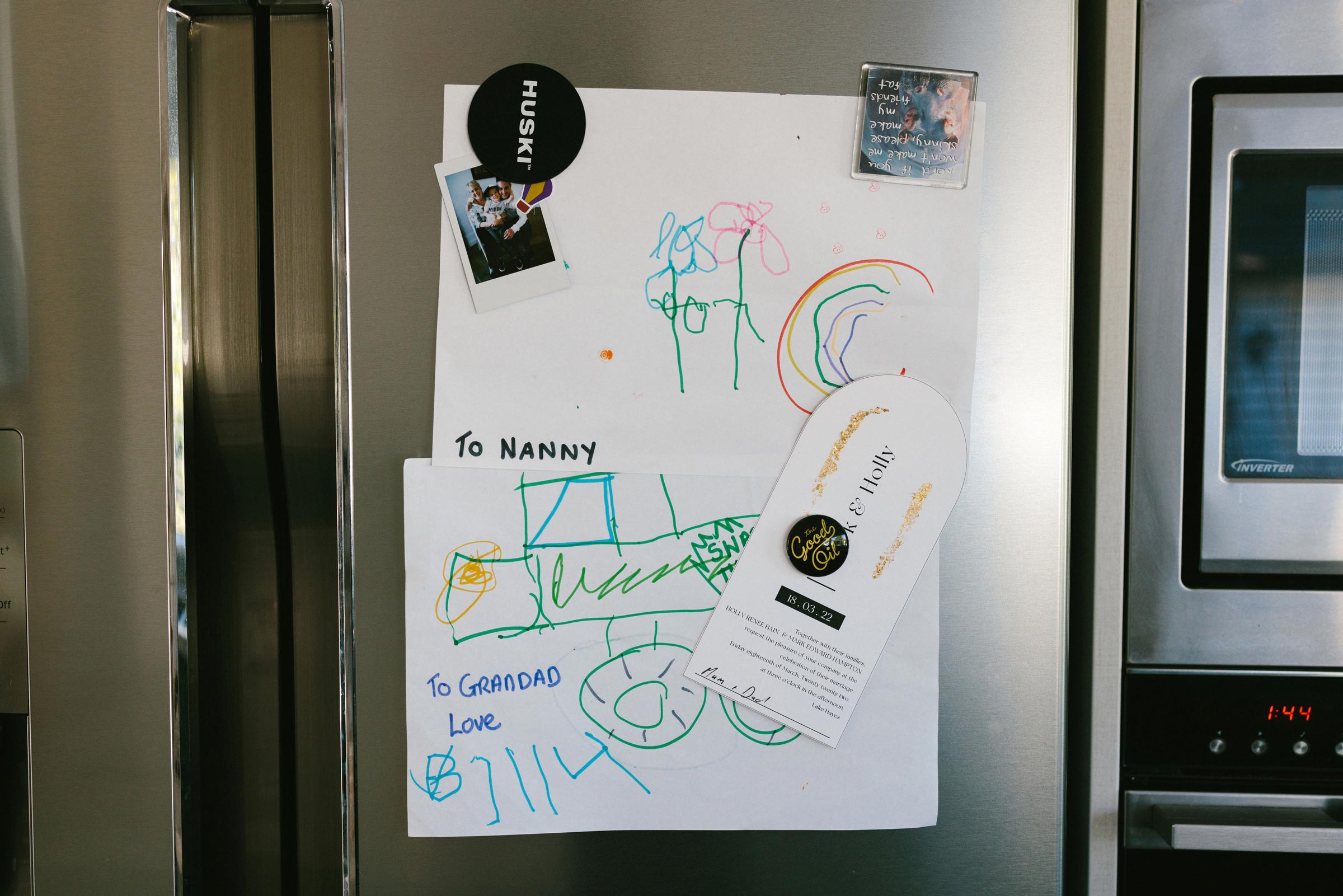
In April, she was blessed with a visit from her grandchildren who live in Melbourne.
“They were almost three and almost five. I had just had chemo two days before they arrived, so if I was tired and on my bed, they would come and snuggle with me. It was just wonderful.”
Janice says she is pouring her energy into staying well and living in the moment but there are still dark moments when she struggles to accept the failings of our health system.
“My husband and I are both public servants. He is a policeman and I’m a nurse and we have worked our entire lives supporting others. I always thought our system would take care of us. Of all of us. And I really hope that in future other people won’t have to go through what I have.”
Janice says people who are unwell shouldn’t have to beg or plead for treatment.
“It’s like death by a thousand cuts. The health system shouldn’t put you in a holding pattern.”

Janice says she has accepted her terminal prognosis because she has no other option. She is looking for the good in life, and continuing to work and enjoy time with friends and family.
“Sometimes I do wonder if sudden death is better than this. I wonder if I had a couple of days to get everyone sorted, whether that would have perhaps been a better way to go. But life doesn’t let you make those choices.”
“And when the time comes, I want to go with dignity and grace, and I don’t want to take my family down with me.”
The reality for Janice and her family is that she has managed to extend her life because she pushed for help.
“I hope the health reforms create major change in our health system because the system is broken. It’s just so very broken.”
“If we hadn’t pushed for help, nothing would have happened. They were just going to let me die.”
Janice says maintaining a quality of life is important to her and she will know when the time comes.
In the meantime, the nurse who has spent decades helping New Zealanders to stay well encourages people to keep seeking treatment, and to keep seeking change in our health system.
“I have to believe our health system will get better. Change has to come.”
Show your support.
Please share Janice’s story.
New Zealand needs access now to modern medicines to treat lung cancer.




Related Stories
Let’s close the Gap
Get Involved1.
REFORM
PHARMAC
Achieve a measurable, political commitment to reform Pharmac and create a fit-for-purpose drug-buying agency that supports and enables greatly improved access to modern medicines – and ensure a direct line of political accountability.
2.
OVERHAUL THE FUNDING
METHODOLOGY
Introduce a globally accepted modern, cost-benefit analysis for medicines and medical devices which looks at the ‘value’ of a medicine, and considers the financial, economic, and social impact of untreated disease on our society.
3.
COMMIT TO AN OUTCOMES-BASED MEDICAL STRATEGY
Develop a Medicines Strategy to guide the decision-making process, create measurable targets to reduce Pharmac’s waiting list, and detail how the agency will respond to rapid developments in modern medicine to improve health outcomes for New Zealanders.